There are basic markers we can measure and improve to gauge overall health.
In a hospital or medical environment, we will measure Heart Rate, Respiration Rate, Temperature, Peripheral Oxygen Saturation (SpO2), Blood Pressure and AVPU (the patients level of alertness).
More invasively, we will then take an ECG and VBG / ABG (Venous Blood Gas / Arterial Blood Gas). These allow us to have a good impression of the current state of your heart and a gross impression of your metabolic processes (glucose, haemoglobin, lactate etc).
With these measures and a good history, we will have a good idea of just how unwell you are and where to start looking for the underlying problem.
If you are unfortunate enough to need admission, part of the nursing process will involve measuring your height and weight. This allows us to calculate the correct drug dose and other supportive measures.
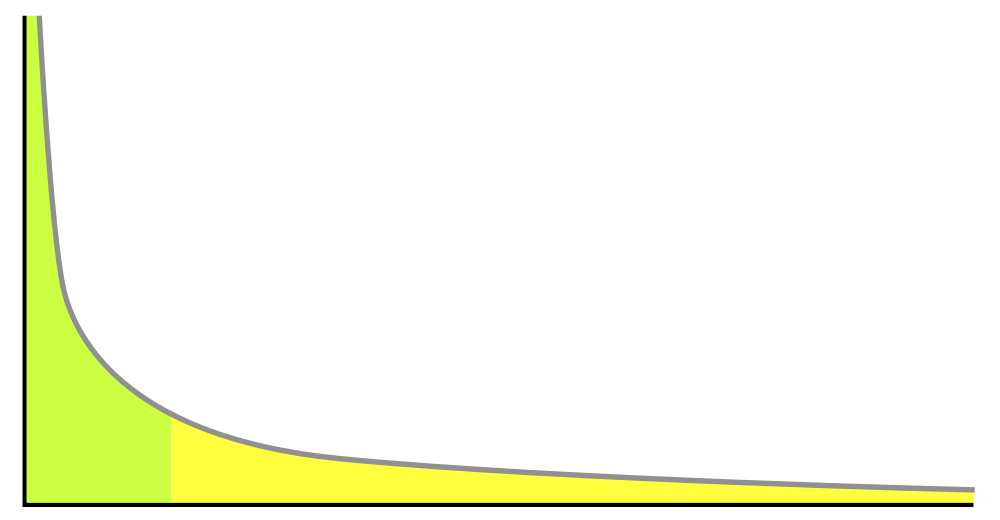
We are also able to calculate your body mass index. This is a commonly used scale, taken from your weight in kilos, divided your height in metres squared. It allows us to quickly see whether you are underweight, average, overweight or obese.
Outside a hospital environment, some of the above measures are often really useful for tracking your personal health, in conjunction with your general practitioner. A low pulse, low blood pressure and stable BMI are all indicators of positive health.
Some people argue that in more athletic individuals, BMI is not a good marker and it may not be very useful in very muscular people. However, it does still indicate how much overall load is being placed on the body, including the heart and the joints.
It can also be argued that, as a healthy adult, until you are able to squat 70-100% of your own body weight, bench press 50-70% of it (dependent on gender), deadlift 120% of your bodyweight, get up from lying on the floor 10 times and walk quickly for at least an hour, with a body fat percentage of between 20 and 25% then you can probably do with losing some fat and improving your global fitness. These are, of course, arbitrary markers for a fully able bodied adult and you may wish to define your own within your own physical boundaries.
Another easy to track health marker is waist to hip ratio. This has been written about before here and is the circumference of your waist, just above the navel, divided by the circumference around your hips. For men, this should be less than 0.9 and for women, less that 0.8. If it were too high then it is indicative of intra abdominal fat, which is known to be unhealthy.
Therefore, I would propose the following as good targets for anyone without underlying known health condition.
A blood pressure of 120-130 / 70
A resting pulse of 50-70bpm
BMI below 25 unless measurably muscular
Waist to Hip ratios appropriate for gender
The above markers for fitness, once warmed up.
If you think that you have a physical restriction holding you back from what you would like to achieve and would like us to support you in improving your health, call and book in for a no obligation chat.
As always, this is not to be taken as legal medical advice and if you have any health concerns, see your registered doctor who will be able to help.

You must be logged in to post a comment.